Human Chorionic Gonadotropin
Human chorionic gonadotropin (HCG) (not to be confused with human growth hormone, or HGH) is a glycoprotein hormone that mimics LH (luteinizing hormone), produced in pregnancy by the developing embryo soon after conception, and later by part of the placenta. Its role is to prevent the disintegration of the corpus luteum of the ovary and to maintain the progesterone production critical for pregnancy in women. It supports the normal development of an egg in a woman’s ovary, and stimulates the release of the egg during ovulation. HCG is used to cause ovulation and to treat infertility in women.
HCG is also used in young boys when their testicles have not dropped down into the scrotum normally. Additionally, HCG is used to increase testicular size after long-term testosterone or anabolic steroid use. However, the latter is an off-label use.
Testosterone replacement therapy triggers the hypothalamus to shut down its production of GnRH (gonadotropin releasing hormone). Without GnRH, the pituitary gland stops releasing LH. Without LH the testes (testicles or gonads) shut down their production of testosterone. For males HCG closely resembles LH. If the testicles have shrunken after long-term testosterone use, they will likely begin to enlarge and start their testosterone production shortly after HCG therapy is instituted. HCG jump-starts your testes to produce testosterone and to increase their size.
HCG can be extracted from pregnant women’s urine or through genetic modification. The product is available by prescription under the brand names Pregnyl, Follutein, Profasi, and Novarel. Novire is another brand but it is a product of recombinant DNA. Compounding pharmacies can also make HCG by prescription in different vial sizes. Brand names of HCG in regular pharmacies cost over $100 per 10,000 IUs. The same amount of IUs cost around $50 in compounding pharmacies. Many insurance policies do not pay for HCG since they consider its use for testicular atrophy while on TRT an off label use. So, most men using it pay for it themselves and get it from compounding pharmacies that sell it a lot cheaper.
HCG is dispensed as a powder contained in vials of 3,500 IUs, 5, 000 IUs or 10, 000 IUs (depending on the compounding pharmacy, these amounts may vary). You can call compounding pharmacies and have them make vials for you with different IU amounts, though. These are usually accompanied by another vial of 1 mL (or cc) of bacteriostatic water to reconstitute the powder into a liquid solution. Bacteriostatic water (water with a preservative that is provided with the prescription) is mixed in with the powder to reconstitute, or dissolve, it before injection. This type of water can preserve the solution for up to 6 weeks when refrigerated. Some patients do not use the 1 mL water vials that come with the commercially (non compounded) available product and instead get their doctors to prescribe 30 cc bottles of bacteriostatic water so that they can dilute the HCG down to a more workable concentration that is more practical for men using lower doses of HCG weekly.
HCG is given as an injection under the skin or intramuscularly (there is still debate on which method is best). The number of IUs per injection will depend on how much bacteriostatic water you add to the dry powder vial. If you add 1 mL to a 5,000 IU powder vial, then you will have 5,000 IUs per mL, so 0.1 mL would be 500 IUs. If you add 2 mL to the 5,000 IU dry powder vial, then you will have 2,500 IUs/mL; 0.1 ml (or cc) in an insulin syringe will equal 250 IUs. If you need to inject 500 IUs, then you inject 0.2 ccs of this mixture. Table 3 provides dilution volumes at different HCG powder/water proportions.
Ultra-fine needle insulin syringes are used to inject HCG under the skin, making this very easy to take even for the needle-phobic. Typical sizes are:
• 1 ml, 12.7 mm long, 30 gauge and
• 0.5 ml, 8 mm, 31 gauge syringes.
Syringes require a separate prescription. Some compounding pharmacies will automatically include them with the shipment, but do not forget to ask them. Never use the syringe that you used for injecting the bacteriostatic water into the powder for injecting yourself; the needle will be dull (I usually use a regular 23 gauge, 1 inch, 3 ml syringe to load up the water). Remember that you also need alcohol pads to clean the injection area and the tip of the vial. Typical injection sites are the abdominal area close to the navel or in the pubic fat pad. Pinch a little of fat on your abdominals and inject into that pinched area, then massage with an alcohol pad. Discard syringes into the sharps container that can be provided by your pharmacy.
As I mentioned before, compounded HCG is a lot cheaper than the commercially available pharmaceutical products. Also, it is sometimes difficult to find commercially available HCG in regular pharmacies.
A review of the literature reveals a wide range of doses of HCG used and that there is very little agreement among physicians. For male infertility, doses range from 1250 IU three times weekly to 3000 IU twice weekly (these studies did not include men on testosterone replacement).
How long does the boost in testosterone last after an injection of HCG? A study looked into that and also tried to determine if high doses would be more effective at sustaining that boost. The profiles of plasma testosterone and HCG in normal adult men were studied after the administration of 6000 IU HCG under two different protocols. In the first protocol, seven subjects received a single intramuscular injection. Plasma testosterone increased sharply (1.6 ± 0.1-fold) within 4 hours. Then testosterone decreased slightly and remained at a plateau level for at least 24 hours. A delayed peak of testosterone (2.4 ± 0.3-fold) was seen between 72–96 hours. Thereafter, testosterone declined and reached the initial levels at 144 hours. In the second protocol, six subjects received two intravenous (IV) injections of HCG (5-8 times the dose given by injection to the first group) at 24-hour intervals. The initial increment of plasma testosterone after the first injection was similar to that seen in the first protocol despite the fact that plasma HCG levels were 5–8 times higher in this case. At 24 hours, testosterone levels were again lower than those observed at 2–4 hours and a second IV injection of HCG did not induce a significant increase. The delayed peak of plasma testosterone (2.2 ± 0.2-fold of control) was seen about 24 hour later than that in the first protocol. So, this study shows that more is not better when dosing HCG. In fact, high doses may desensitize Leydig cells in the testicles. It also showed that testosterone blood levels peak not once but twice after HCG injections. I wish they had studied a lower dose than 6000 IU since very few physicians prescribe this high dose.
HCG may not only boost testosterone but also increase the number of Leydig cells in the testicles. It is well known that Leydig cell clusters in adult testes enlarge considerably under treatment with HCG. However, it has been uncertain in the past whether this expansion involves an increase in the number of Leydig cells or merely an enlargement of the individual cells. A study was performed in which adult male Sprague-Dawley rats were injected subcutaneously daily with 100 IU HCG for up to 5 weeks. The volume of Leydig cell clusters increased by a factor of 4.7 during the 5 weeks of HCG treatment. The number of Leydig cells (initially averaging 18.6 x 106/cm3 testis) increased to 3 times the control value by 5 weeks of treatment (P<0.001), while the average volume of individual Leydig cells (initially ~2200 µm3) enlarged only 1.6 times. They concluded that chronic treatment with HCG increases the number of Leydig cells in the testes of adult rats. We do not know if these results can be extrapolated to men.
Currently there are no HCG guidelines for men who need to be on testosterone replacement therapy and want to maintain normal testicular size. A study that used 200 mg per week of testosterone enanthate injections with HCG at doses of 125, 250, or 500 IU every other day in healthy younger men showed that the 250 IU dose every other day preserved normal testicular function (no testicular size measurements were taken, however). Whether this dose is effective in older men is yet to be proven. Also, there are no long-term studies using HCG for more than 2 years.
Due to its effect on testosterone, HCG use can also increase estradiol and DHT, although I have not seen data that shows if this increase is proportional to the dose used.
So, the best dose of HCG to sustain normal testicular function while keeping estradiol and DHT conversion to a minimum has not been established.
Some doctors are recommending using 200–500 IUs twice a week for men who are concerned about testicular size or who want to preserve fertility while on testosterone replacement. Higher doses, such as 1,000–5,000 IUs twice a week, have been used but I believe that these higher doses could cause more estrogen and DHT-related side effects, and possibly desensitize the testicles for HCG in the long term. Some doctors check estradiol levels a month after this protocol is started to determine whether the use of the estrogen receptor modulators tamoxifen (brand name: Nolvadex) or anaztrozole (brand name: Arimidex), is needed to counteract any increases in estradiol levels. High estradiol can cause breast enlargement and water retention in men but it is important at the right blood levels to maintain bone and brain health.
***************************************************************
Shippen’s Chorionic Gonadotrophin Stimulation Test (for males under 75 years of age)
Even though there seems not be an accepted and clinically proven protocol to dose HCG, Dr. Eugene Shippen (author of the book “The Testosterone Syndrome”), has developed his own after his own experiences. Most doctors do not follow this protocol but I am showing it here since I get a lot of questions about it. I have never used this protocol myself since I have been on testosterone replacement for over 15 years.
Dr. Shippen has found that a typical treatment course for three weeks is best for determining those individuals who will respond well to HCG treatment. It is administered daily by injection 500 units subcutaneously, Monday through Friday for three weeks. The patient is taught to self administer with 50 Unit insulin syringes with 30 gauge needles in anterior thigh, seated with both hands free to perform the injection.
Testosterone, total and free, plus E2 (estradiol) are measured before starting the protocol and on the third Saturday after 3 weeks of stimulation (he claims that salivary testing may be more accurate for adjusting doses). Studies have shown that subcutaneous injections are equal in efficacy to intramuscular administration.
By measuring the effect on his HCG protocol on total testosterone, he identifies candidates that require testosterone replacement versus those who just require having their testicles “awaken” with HCG to produce normal testosterone. I am yet to see any data that substantiates his approach, however.
Here is how he determines Leydig (testicular) cell function:
1. If the HCG protocol causes less than a 20% rise in total testosterone he suggests poor testicular reserve of Leydig cell function (primary hypogonadism or eugonadotrophic hypogonadism indicating combined central and peripheral factors).
2. 20-50% increase in total testosterone indicates adequate reserve but slightly depressed response, mostly central inhibition but possibly decreased testicular response as well.
3. More than 50% increase in total testosterone suggests primarily centrally mediated depression of testicular function.
He then offers these options for treatment for patients depending on the response to HCG and patient determined choices.
1. If there is an inadequate response, then replacement with testosterone will be indicated.
2. The area in between 20-50% will usually require HCG boosting for a period of time, plus natural boosting or “partial” replacement options.
I am yet to see what he means with natural boosting!
Dr. Shippen believes that full replacement with testosterone is always the last option in borderline cases since improvement over time may frequently occur as the testicles’ Leydig cell regeneration may actually happen. He claims that much of this is age dependent. Up to age 60, boosting is almost always successful. In the age range 60-75 is variable, but will usually be clear by the results of the stimulation test. Also, disease related depression of testosterone output might be reversible with adequate treatment of the underlying process (depression, obesity, alcohol, deficiency, etc.) He claims that this positive effect will not occur if suppressive therapy is instituted in the form of full testosterone replacement.
3. If there is an adequate response of more than 50% rise in testosterone, there is very good Leydig cell reserve. HCG therapy will probably be successful in restoring full testosterone output without replacement, a better option over the long term and a more natural restoration of biologic fluctuations for optimal response. But I am yet to see any data on long term use of HCG used in this approach! (I invite researchers to do such studies)
4-. Chorionic HCG can be self-administered and adjusted according to response. In younger, high output responders (T > 1100ng/dl), HCG can be given every third or fourth day. This also minimizes estrogen conversion. In lower level responders (600-800ng/dl), or those with a higher estradiol output associated with full dose HCG, 300- 500 units can be given Mon-Wed-Fri. At times, sluggish responders may require a higher dose to achieve full testosterone response.
Dr. Shippen believes in checking salivary levels of free testosterone on the day of the next injection, but before the next injection to determine effecacy and to adjust the dose accordingly. He claims that later as Leydig cell restoration occurs, a reduction in dose or frequency of administration may be later needed.
5. He recommends to monitor both testosterone and estradiol levels to assess response to treatment after 2 - 3 weeks after change in dose of HCG as well as periodic intervals during chronic administration. He claims that salivary testing will better reflect the true free levels of both estrogens and testosterone. (Pharmasan.com and others) Most insurance companies do not pay for salivary testing. Blood testing is the standard way to test for testosterone and estradiol.
6. Except for reports of antibodies developing against HCG (he mentions that he has never seen this problem), the claims that there are no adverse effects of chronic HCG administration.
Dr.Shippen’s book was published in the late 90’s. I know of no physician that uses his protocol. I have no opinion on its validity. The idea that testicular function can be improved with cycles of HCG in men with low testosterone caused by sluggish yet functioning Leydig cells is an interesting concept that needs to be studied. I guess that since this protocol requires very close monitoring, many doctors have avoided using it. The off label nature of the protocol’s use of HCG can also make it expensive for patients who will have to pay cash for its use and monitoring.
A very well known doctor in the field of testosterone replacement, Dr. John Crisler (www.allthingsmale.com), recommends 250 IU of HCG twice per week for all TRT patients, taken the day of, along with the day before, the weekly testosterone cypionate injection. After looking at countless lab printouts, listening to subjective reports from patients, and learning more about HCG, he reports to be shifting that regimen forward one day. In other words, his patients who inject testosterone cypionate now take their HCG at 250 IU two days before, as well as the day immediately previous to, their weekly intramuscular shot. All administer their HCG subcutaneously, and dosage may be adjusted as necessary (he reports that rarely more than 350 IU twice weekly dose is required).
For men using testosterone gels, the same dose every third day has anecdotally helps to preserve testicular size (the dose of the gel has to be adjusted after a month of HCG to compensate for the increased testosterone caused by HCG).
Some doctors believe that stopping TRT for a few weeks in which only 1000- 2000 IU HCG weekly is used provides a good way to stimulate testicular function without having to use HCG continuously. I have not seen any data to support this approach. Others believe that cycling HCG on and off while maintaining TRT may prevent any desentization of testicular Leydig cells to HCG. Again, no data or reports have been published on this approach.
Some men have asked me why we cannot use HCG solely to make our own testicles produce testosterone without the use of TRT along with it. According to Dr. Crisler, using HCG as sole testosterone replacement option does not bring the same subjective benefit on sexual function as pure testosterone delivery systems do—even when similar serum androgen levels are produced from comparable baseline values. However, supplementing the more “traditional” transdermal, or injected options, testosterone with the correct doses of HCG stabilizes blood levels, prevents testicular atrophy, helps rebalance expression of other hormones, and brings reports of greatly increased sense of well-being and libido. But in excess, HCG can cause acne, water retention, moodiness, and gynecomastia (breast enlargement in men).
Many men have complained that their doctors do not know about HCG and how to use it (I do not blame doctors for being confused!). Some spend a lot of time trying to find doctors to feel comfortable prescribing it. One good way to find out what doctor in your area may be currently prescribing it is to call your local compounding pharmacies to ask them what doctors call them for their patients’ prescriptions.
If you decide (with the agreement of your doctor) that you want to use HCG with your TRT regimen at 500 IU per week, then you will need 2000 IU per month. I personally do not like to have diluted HCG sitting in my fridge for over six weeks (HCG may degrade with time after mixed in with bacteriostatic water even when refrigerated). So, a 3000 or 35000 IU vial should suffice for 6 weeks.
Your doctor can call in the following prescription to a compounding pharmacy:
Human Chorionic Gonadotropin, 3500 IU (or any other IU amount) vial, #1, 3 refills, as directed
Every 5 weeks, remember to call the compounding pharmacy to get the next shipment of HCG so that you do not run out.
After reading this section, you probably agree with me that using HCG requires a lot of discipline since you have to remember to inject it weekly in addition to your weekly or bi-weekly testosterone injection. But I know of many men who have that type of commitment since they do not want testicular size reduction. And many of us may just be fine with our reduced testicular size as long as testosterone is actually doing its job in improving our sex drive. And some lucky men do not get testicular atrophy at all on testosterone (those with large testicles to start with usually do not seem to complain about shrinkage as much as men starting with smaller testicular size before TRT). So it is a personal decision at the end!
As you will read in the section “HPGA dysfunction” HCG is also used in a protocol in combination with clomiphene and tamoxifen to attempt to bring the body’s own testosterone production back to normal when someone needs to stop testosterone or anabolic steroids after long-term use. This protocol only works for those who started testosterone or anabolic steroids at normal baseline testosterone levels (bodybuilders and athletes) and it is not intended to work in those of us who had testosterone deficiency (hypogonadism) to start with.
As you can tell, there is no agreement on the correct dose and frequency of HCG. I really hope that researchers in the endocrine field compare different protocols in a controlled manner so that we can settle this issue once and for all. I encourage pharmaceutical companies to seek approval for using HCG for prevention of testicular atrophy in men using TRT. This new indication can prove to be lucrative as the TRT market grows over 2 billion dollars a year in the United States as more men become aware of hypogonadism treatment options.
PERSONAL COMMENT: I have used HCG to reverse testicular shrinkage and it works extremely well not only for that purpose but also for boosting sex drive. I do have to remind myself that as soon as I stop using it, testicular atrophy will recur. I have recently started using it in small doses (250 IU twice a week subcutaneously) which seems to be a good maintenance regimen for me. I get my HCG from compounding pharmacies at $70 per 10,000 IUs since the pharmaceutical commercial products are too expensive and rarely paid by insurance for testicular atrophy. I remind men that HCG can increase your estradiol and DHT blood levels, so it is important to have your doctor retest you for both of these values after you start. Lowering testosterone dosage may be required when using HCG along side with TRT since HCG can have an additive effect on testosterone blood levels. But we need so much more data on HCG to stop making assumptions and using protocols that are endorsed by anecdotal information.
Patient Price for HCG is $30-$70 depending on the number of IUs.



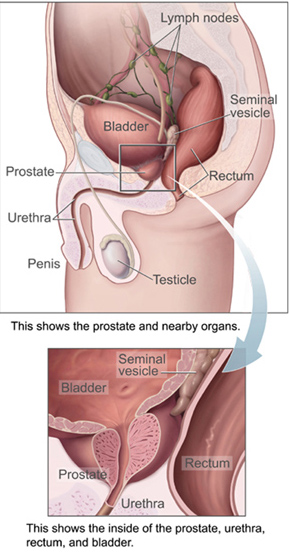 Prostate cancerThis little gland attracts a great deal of attention in men’s health. One of the major issues is related to cancer. Prostate cancer is one of the leading causes of death in men in the United States. As men age, small hidden prostatic lesions become increasingly common. These may or may not become cancerous. These lesions occur in 30 percent of American men over the age of 45, with the prevalence rising to more than 80 percent for men over the age of 80. Genetic factors and life style conditions such as diet are believed to contribute to this transformation. [Figure 14.The prostate and surrounding organs (Courtesy of Wikipedia.com)]
Prostate cancerThis little gland attracts a great deal of attention in men’s health. One of the major issues is related to cancer. Prostate cancer is one of the leading causes of death in men in the United States. As men age, small hidden prostatic lesions become increasingly common. These may or may not become cancerous. These lesions occur in 30 percent of American men over the age of 45, with the prevalence rising to more than 80 percent for men over the age of 80. Genetic factors and life style conditions such as diet are believed to contribute to this transformation. [Figure 14.The prostate and surrounding organs (Courtesy of Wikipedia.com)]



